With all the unknowns currently in front of us as we work to reach the “new normal” or “next normal”, there are a few things we can expect:
- The new/next normal will NOT look like the old normal
- Team alignment and connectedness will be more important than ever, yet to achieve it, we can’t count on physical connectedness.
We are physically and socially disconnected in a way we have never experienced before. Emotional Connectedness will fill that void, and organizations who take the right approach can and will achieve a level of alignment that exceeds what they had before.
For many people, a return to normal means the comfort of homemade chicken soup and freshly made bread. However, any return to normal in pandemic conditions will only prove regressive. Any return to normal means a return to complacent steps backward to recreate something remembered. It shouldn’t happen, and it ain’t gonna happen!
Healthcare workers, paramedics, and tens of millions impacted directly or indirectly by COVID-19 have moved past thinking of comfort food. They must accept the devastating hand they have been dealt, but they can design a resilient future shaped by their experience, suffering, and loss. Professionals, workers, service providers, and consumers everywhere would profit by looking beyond the normal.
This pandemic has tested our social connectedness severely. People have died alone. Multiple millions have been ordered to stay in place. Millions are unemployed. And, doctors, nurses, and hospital staff have quarantined themselves from their families and worked sequential 12- to 20-hour days without rest.
Committed “to do no harm,” they find themselves making mind-altering decisions in triage. It tears at them apart — physically and emotionally. Still, they are urged at one time to socially separate and fight this together.
What will it take to put them together again?
Warlike conditions exploit separation. As people separate, they increase their vulnerability. But the human social instinct to connect emotionally — even over great distances — will drive a new future if it is enabled, empowered, and energized to do so.
Any observation of the behavior of healthcare workers, for instance, sees them coalescing as strong teams despite group and individual existential threats. They leverage positive deviance to address the absence of personal protective equipment. And, they provide solace to patients dying without family nearby. They continue to be exemplars of the resilience wrought by emotional connectedness and their results-based culture.
Five physician partners founded Springfield Clinic in 1939 to serve the healthcare needs of residents in downstate Illinois. Today, 450 physicians and advanced practitioners serve a million citizens throughout central Illinois. Its 2,400 employees reach 40 destinations and support patients in eighty medical specialties and subspecialties. The award-winning clinic has a clear vision:
“Springfield Clinic is a progressive physician-led organization devoted to providing the highest quality health care to our patients. The Clinic’s goal is to be a nationally recognized leader in the delivery of value-driven, coordinated patient care through service excellence, innovation and optimal health outcomes.”
It aspires to national recognition and identifies the key performance indicators: value-driven, coordinated care, service excellence, innovation, and optimized health outcomes. Each metric relates to the others; none acts independently of the others.
Now, Springfield Clinic operates far from the dense experience of New York hospitals. However, it has mastered the challenge of managing crises over multiple remote locations to confirm its role as a “Community of Caring.” According to Jack O’Hara, Springfield Clinic’s Chief Information Officer, “we’re in a great financial position, we’re in a great position from a people standpoint and our positive vision of the future looks very bright right now.”
He credits the Results Based Culture Change Process for boosting the organization’s character and performance. O’Hara notes, “It’s been really, really exciting to work with Louis Carter to move Springfield Clinic towards a top echelon business.”
Working remotely and in-person with Springfield’s executive team, we were able to strengthen Jack O’Hara and his peers with a process he thoroughly enjoyed and came to value highly.
4 Process for Change – The Next Practice Change Model
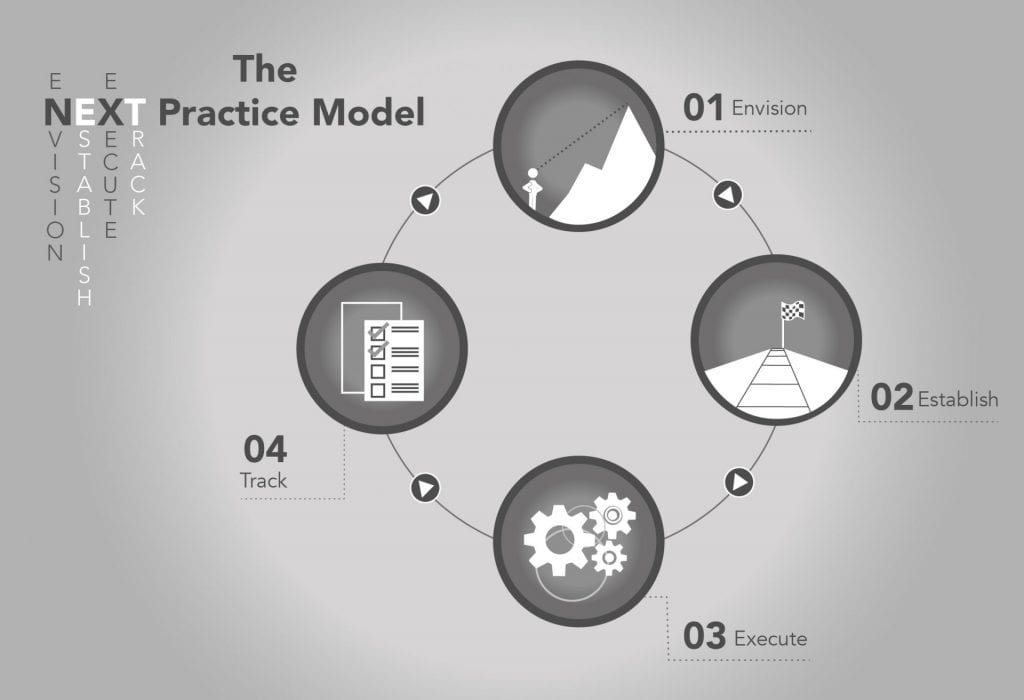
1. Envision: We cannot reach a goal we cannot see. The goal must have dimension, vibrance, and tangibility. It must be within reach, close enough for us to see and desire. But any transformation starts at the top where key stakeholders join the CEO and leadership team to create a culture map.
In Springfield Clinic’s case, CEO Ray Williams invited Louis Carter to work closely with him and their decision-makers to co-create the blueprints for establishing baselines, to set and align goals, and to identify results-based metrics. But framing and informing the vision meant inspiring a new culture.
2. Establish: Developing a results-based culture begins with understanding the practice of co-creation. Jack O’Hara described it as a “laboratory” where the leadership team talked about the strategic direction for Springfield Clinic. Over several session, they shared input on questions including:
• What is going on in the world?
• What are the existential threats?
• What could happen?
• What do we know about the local and distant competition?
• What do we want to be as a multiple location clinic?
• What do we want to be as a regional business?
In this phase, co-creation sessions are held that excite the hearts and minds of participants to stir accountability throughout the organization.
O’Hara explained, “we connected our mission to our strategic initiatives; then, we connected that down to the specific executive’s goals for this year.” With agreement on objective and key results, the leaders took the understanding to their senior teams with project management tools to deliver promise at the granular level.
A results-based culture enables opportunities for everyone in the organization to voice the change on which they want to build the envisioned future. The common purpose increases trust and understanding. It lays the foundational support for reaching established goals while identifying inhibitors and roadblocks that might curtail adoption.
3. Execute: When John O’Hara accepted his position some six months before our meeting, the water cooler conversation centered on the constantly shifting priorities at Springfield Clinic. “Now,” he said,” we essentially have a master list of how we’re going to complete our strategic directions. For example, with accountability, everybody knows what they have to do.” They label nothing a priority unless it aligns with strategic goals unless everyone knows what they must do and unless it will lead to a high level of success.
Maps remain paper, after all, until something moves along its paths. Maps require supportive action plans enabling movement and metrics to improve behavior. This requires specific attention on the identified enablers and inhibitors, one that allows everyone to silence the noise with a clear focus on what is needed to align and achieve shared goals.
Jack remembers holding a session with his Information Technology Team where they talked about how they could work better together but more specifically how he could do better as CIO. Teams in breakout sessions asked, “Hey, what are the things that Jack, as a Chief Information Officer, needs to do better?” That feedback revealed what the frontline staff feels, how it feeds through their managers and directors to the C-suite executives directing the organization’s strategy.

4. Evaluate: If cannot measure it, it has not happened. Rather than rely on counting alone, the Carter Change Method uses Agile, adaptive, and adjustable tools to assess and value the results of the executed change. When these indicators report negative variances from anticipated goals, Carter and teams revisit the execution to analyze the gaps and make the adjustments to regain the traction to move forward.
This calls for a “Reinvention Room” where team members measure how they did with what they set out to do. Any evaluation finds positive, neutral, and negative variances from the aspiration. The Re-invention Room offers the physical and psychological opportunity to map the next steps to sustain the positive, energize the neutral, and correct the negative with necessary adjustment and adaptation.
Helping Springfield Clinic Work
A Results Based Culture has helped Springfield Clinic find itself, set its priorities, and appreciate results-based thinking. Its executive team finds itself engaged and energized, focused and committed. They have taken their work and molded so it makes it right and comfortable for individual team members, helping them create their own excellence. They now value their interdependence, their connectedness in co-creation of projects, plans, and performance aligned with the organization’s vision. And, they have done this successfully — across multiple locations and thousands of employees many of whom connect remotely. They have the resilience to survive this pandemic and beyond.